Acne – Your Complete Guide to Clear Skin

ACNE
Acne is one of the most common inflammatory skin disorders. It affects a wide range of people worldwide, and is seen in individuals of almost all ages and backgrounds. I see patients suffering from acne ranging from 10 – 40 years old, who feel that they have tried everything under the sun with no luck in solving the issue, or who have scarring or discolouration of the skin as a result of the breakouts. Battling acne can have a huge impact on a person’s self esteem, and effective treatment can change lives.
There are a number of elements that contribute to acne, such as hormones, genetics, lifestyle, and skin care. Determining and treating the cause of acne is essential to achieve long term results, and to do so we need to look at the skin on a physiological level.
THE ORIGINS OF ACNE
So how does acne occur? The skin contains many units called pilosebaceous units, which are composed of a hair follicle, the hair shaft and the sebaceous gland. Sebum, an oily secretion essential for skin integrity, is produced by the sebaceous gland, and then moves up to the surface of the skin with shedding skin cells.
Patients with acne are highly sensitive to androgen (male sex) hormones, which cause increased sebum production and abnormally fast skin cell turnover. This excessive activity essentially forms a ‘plug’ in the pilosebaceous unit, building congestion and providing a breeding ground for bacteria, namely P. Acnes bacteria.

Stage 1
Androgenic hormones influence the amount of sebum (oils) produced by the sebaceous gland. The sebum binds together dead skin cells and other matter causing a blockage, as well as a fertile environment for bacteria.
Stage 2
The colonisation of P. acnes bacteria initiates inflammation
Stage 3
Fast skin cell turnover (keratinisation) occurs not only on the surface of the skin, but also within the follicle, further adding to congestion.
DOES ACNE ONLY AFFECT TEENAGERS?
In short, no. It is normally around the age of 12 to 15 years, when our hormones start firing up, that acne can make its debut. Peak severity tends to be between 17 and 21 years of age. Most of the time, our hormones even out on their own and acne clears up by the age of 25.
However, acne is becoming an increasingly common problem in patients over 25 years of age, particularly in women. In some cases, acne can persist in patients up to the age of 45.
WHAT FACTORS AFFECT ACNE?
A number of contributing factors can exacerbate acneic skin conditions, so it is important to assess all aspects of one’s life when treating acne. These factors include:
Family History: If your parents have a history of severe acne during puberty, is it likely to be passed on to the children.
Medical History: Conditions affecting hormonal regulation such as Polycystic Ovary Syndrome, Congenital Adrenal Hyperplasia and Cushing’s Syndrome can contribute to the onset or worsening of acne.
Medications: Regular medications such as iodides, bromides and steroids can have an effect on acneic skins. A full list of medication can be found here.
Hormones: Increased sebum production due to androgens acting on the sebaceous gland is a factor amongst nearly all acne sufferers. Acne flare ups during the menstrual cycle are also common in many women.
Lifestyle factors: Acne can flare during times of stress and there is emerging research on diet and acne. High inflammatory diets (resulting in excess insulin release) including gluten, dairy and sugar can contribute but do not cause acne.
Cosmetics: The use of oily and cream based cosmetics and skin care products can promote plugging of the pilosebaceous unit and result in comedone formation.
Other: Heat, friction and trauma to the skin can also exacerbate the condition.
BUT WHY DO I ONLY GET ACNE ON MY FACE / BACK / CHEST?
Acne is the result of over activity of the sebaceous glands. Because of this, it makes sense that lesions present in areas with a high density of these glands. The areas most commonly affected by acne are the face, upper back and chest, however the neck, shoulders, lower back and buttocks may also be affected.
TYPES OF ACNE
Acne can be classified into 3 categories. Severity is graded according to the number and type of lesions on the skin.
Mild: Typically limited to the face. Closed and open comedones, with few inflamed lesions
Moderate: Increased number of inflammatory papules and pustules on the face
Severe: Nodules and cysts are present.
TREATMENT
Through understanding the cause of acne, we can look at what needs balancing in the skin, including hydration and water levels, clearing of bacteria and congestion, regulation of cell renewal and oil flow, and exfoliation of the surface skin cells.
Acneic skin generally has quite an impaired barrier function, meaning that it is actually lacking water and can be quite sensitive. In saying this, it is SO important to use home care products that are yes, effective in clearing congestion and regulating oil, but also that are going to replenish and protect the skin. Stripping the skin will only cause oil glands to flare up even more in retaliation.
IN CLINIC
In clinic, medical peels, Acnelan, or treatments such as the Hydrafacial containing active ingredients to soften and dissolve the skin and control oil flow is an effective and gentle way to clear congested skin. Pairing these treatments with Healite therapy, to kill off the p.acnes bacteria and encourage skin healing further speeds up results.
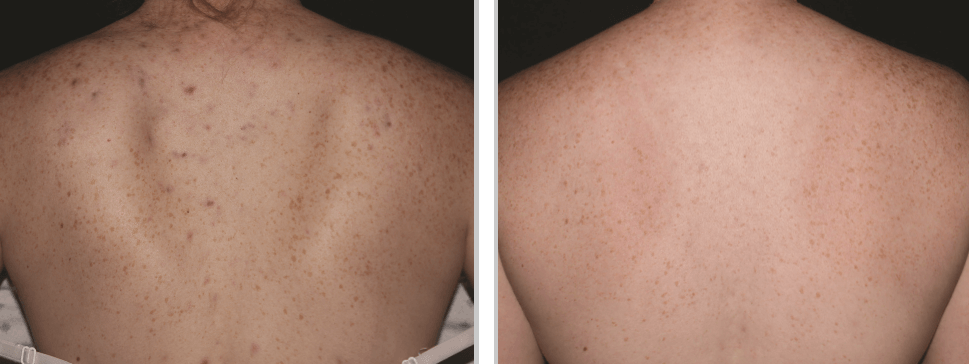
Another treatment that I have been blown away by is the BBL Forever Clear, which provides a photochemical and photothermal effect on the skin, not only killing bacteria but assisting in lightening of pigmentation scarring. Alternating BBL treatments to kill bacteria and strengthen the skin, with Hydrafacial therapy to extract, exfoliate and hydrate the skin is an incredible program with phenomenal results.
AT HOME
Regular home care using products with active ingredients such as Lactic and Mandelic Acid, which gently exfoliate and break down bonds between the skin cells, whilst adding hydration at the same time is a fantastic way to open up any congested pores.
Including Salicylic acid in your skin care regime will help to balance the oil flow as well as provide an antibacterial effect.
I could go on and on about the benefits of Retinol in skin care, but in this instance I’ll refine it in relation to acne. Regular use of topical Retinol is key for regulating skin cell renewal and keratinisation. Retinol is a derivative of Vitamin A that works on the dermal level of the skin, where the skin’s factory lies. Think of it as a traffic instructor for your skin, preventing “traffic jams”, or in other words the congestion that happens when hyperkeratosis occurs. This in turn prevents the buildup of skin cells that can cause blockages.
Retinol also has an antibacterial effect on any underlying p.acnes bacteria, regulates the activity of the sebaceous gland, activates hydration in the epidermis of the skin, and allows for better penetration of other active ingredients.
When introducing any Vitamin A derivative to the skin, it is important to do so slowly, and restrict use to night times only with the use of antioxidants and SPF 50+ during the daytime.
It is so important to remember that when treating acne it almost certainly will get worse before it gets better. This is referred to as the purging period, and is a result of exfoliation of the skin that was trapping everything underneath, and encouraging congestion to come up to the surface so it can be cleared away to reveal the new, healthy, balanced skin underneath.
SCARRING AND HYPERPIGMENTATION
We are all guilty of a little DIY extraction, even though we KNOW it’s a bad idea and that it never works out in our favour. Unfortunately, these habits can lead to scarring and pigmentation changes to the skin that can last for months or years.
Hyperpigmentation occurs when too much melanin is created on the skin’s outer layers. Usually this extra melanin production happens when your skin is trying to heal or protect itself as a response to inflammation caused by stress to the skin, such as the inflammation caused by pimples/congestion, as well as squeezing and scratching. Pigmentation resulting from acne scarring can be treated with a number of active cosmeceutical ingredients that lighten pigment and inhibit melanin production, as well as BBL photorejuvenation.
Acne scarring can also take the form of pitting and textural changes in the skin. There are several different types of acne scarring including
Boxcar Scars: Shallow with sharp edges
Icepick Scars: Deeper, narrow and severe scars
Keloid Scars: Discoloured, bumpy, raised and generally hard to touch
Rolling Scars: Wavy and shallow
These types of scars result from collagen fibres not being able to sufficiently restore the skin after injury, leaving depressions and irregularities of the surface texture. There are a number of treatments including skin needling and in some cases TCA cross that are very effective in restoring scarring.
It is important to note that scar revision can only be done once the initial congestion and inflammation has been treated, as spreading bacteria across the skin is the last thing we want to do.
As you can see, there are so many contributing factors to the onset and persistence of acne, as well as a number of conditions that may result as aftermath of inflammation. The best way to begin your skin journey is to have a consultation with a full skin analysis, so that a comprehensive and personalised treatment plan can be put into place.
With our extensive range of medical grade treatments and technology, there are a number of ways to tackle acne from every direction, and provide our patients with long term results.